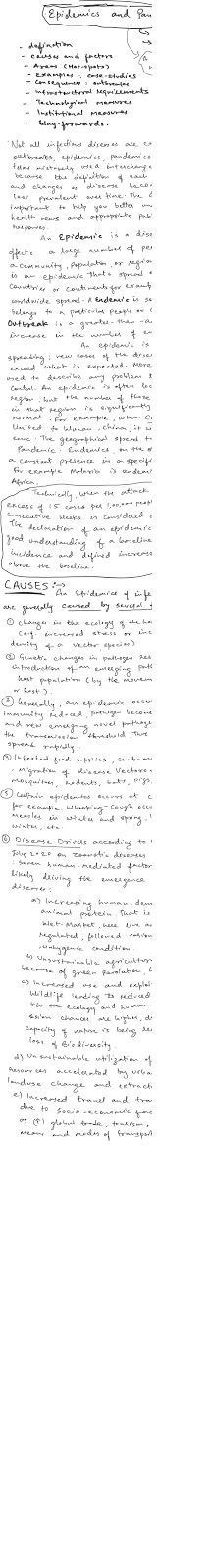
Pandemics and Epidemics in world and India :---
===============================
History of world diseases and infection spreads at above the normal level called by different names as per degree of infections such as
1) outbreaks :- when it occurs over the area.
2) Epidemics :- when spread is over a particular geography only
3) Pandemics :-when spread cover across country or world.
Examples of deadly disease and infections causing death to millions of people in different parts of world are given below :-
History of pandemic in the world :---
====================
Name,Time period,Type / Pre-human host , Death toll
1)Antonine Plague 165-180---Believed to be either smallpox or measles-5M
2)Japanese smallpox epidemic 735-737 ,Variola major virus1M
3)Plague of Justinian, 541-542 Yersinia pestis bacteria / Rats, fleas30-50M
4) Black Death 1347-1351 Yersinia pestis bacteria / Rats, fleas 200M
5) New World Smallpox Outbreak 1520 – onwards Variola major virus 56M
6) Great Plague of London 1665 Yersinia pestis bacteria / Rats, fleas100,000
7) Italian plague 1629-1631 Yersinia pestis bacteria / Rats, fleas1M
8) Cholera Pandemics 1618-1923V. cholerae bacteria1M+
9) Third Plague 1885 Yersinia pestis bacteria / Rats, fleas12M (China and India)
10) Yellow Fever Late 1800s Virus / Mosquitoes 100,000-150,000 (U.S.)
11) Russian Flu 1889-1890 Believed to be H2N2 (avian origin)1M
12) Spanish Flu1918-1919 H1N1 virus / Pigs 40-50M
13) Asian Flu1957-1958H2N2 virus1.1M
14) Hong Kong Flu 1968-1970 H3N2 virus1M
15) HIV/AIDS 1981 -presentVirus, Chimpanzees 25-35M
16) Swine Flu 2009-2010, H1N1 virus / Pigs 200,000
17) SARS 2002-2003 Coronavirus / Bats, Civets770
18) Ebola2014-2016 Ebolavirus / Wild animals11,000
19)MERS2015-Present Coronavirus / Bats, camels 850
20)COVID-192019-PresentCoronavirus – Unknown (possibly pangolins)11,400 (as of Mar 20, 2020)
Causes for such spreading of deadly diseases are :--
=============
1) Demographic factors such as high population size, density, and growth, age structure, etc
2) Health infrastructure bottlenecks like shortages of hospitals, health equipments, health personals.

According to global disease hotspot 2.0 by ecohealthalliance , the disease hotspot world map first time published in 2008 see below:

As you can see, the map identifies parts of South and Southeast Asia, West and Central Africa, and Latin America as having the highest potential for disease spillover. Places like Bangladesh, India, and China are the brightest, indicating highest risk. That is for several reasons, first of all these are some of the fastest growing countries worldwide; Bangladesh is currently one of the most densely populated countries in the world. These nations are also heavily forested–India and China–being two of the ten most forested areas in the world–and in a lot of cases, that forest is being razed to extend urban centers or further agricultural production. It is conditions like these that create high potential for disease to spill from wildlife populations into humans (or vice versa, though the hotspots map only tracks spread of disease in one way). Zoonotic diseases which emerged in Southeast Asia and have jumped to humans include SARS, bird flus, and Nipah virus.

Case studies of epidemic and pandemic in the world :
COVID 19 :
H1N1
Ebola
Saras
MERS
India’s Epidemics situation is worse, recurrent, causing death to millions of people, heavy economic loss, etc every year from dengue, malaria Japanese encephalitis, India’s distinctive demographic profile and geographic position presents a unique challenge to infectious disease management. The country is one of the world’s most populated nations, with a substantial proportion of the population living in impoverished areas where infectious diseases can spread exponentially (1, 2). Geographically, the country lies within the distribution zone of important disease vectors such as the Aedes aegypti mosquito (which spreads dengue and Zika virus), and the country is subject to annual monsoon seasons which perpetuate mosquito borne diseases such as Dengue, Japanese Encephalitis and Chikungunya (3).
In 2015, India saw its largest recorded dengue outbreak, with national authorities confirming almost 100,000 cases and 220 deaths (almost double that of the preceding year) – the actual number of cases and deaths are expected to be much higher with underreporting and surveillance a known issue in India (1, 4, 5). The 2015 dengue outbreaks in India gained considerable international attention, with reports of public and private hospitals overrun with dengue patients, bed-sharing, and hospitals having to turn away sick patients, which led to a controversial decision to cancel leave for doctors and paramedical staff (1, 5, 6). With the 2016 monsoon expected to be heavier than last year’s, there is an expectation of even more cases of mosquito borne disease (5). So far this year 180 dengue cases have been reported, in addition, a chikungunya epidemic is suspected to be occurring, however a lack of facilities capable of confirming chikungunya infection, means that the epidemic in unlikely to be officially reported
(7).
Recurrent epidemics of encephalitis (inflammation of the brain) of unknown cause have also occurred in India (8). Between 2008 and 2014, there have been more than 44,000 cases and nearly 6,000 deaths from encephalitis in India, particularly in Uttar Pradesh and Bihar. This year has also seen a rise in encephalitis, over 125 children reported to have died in Baba Raghav Das Hospital, Gorakhpur alone, with nearly 400 children being treated for the disease (9, 10). As a response to these figures, there has been a recent push for encephalitis to be the list of national notifiable diseases (9-11). It is also critical to identify the virus or pathogen causing these large outbreaks.
The pandemic strain of influenza A(H1N1) cases in India caused a major epidemic since 2012, with 39,000 cases and 2500 deaths reported in 2015, (compared to 1000 cases and 218 deaths reported the preceding year) (12, 13).Following the 2009 pandemic, India saw a resurgence of this virus in the 2012-13 winter, and a progressive worsening resurgence since December 2014. The death rate in India was vastly higher than other countries, over 6% compared to global death rate of 0.02% in 2009. Hospitals and clinicians reported much more severe influenza disease than they had seen previously, confirmed the very high mortality.
Questions have arisen about whether the virus in India had mutated to cause such severe disease, but genetic information is very sparse, and there is an urgent need for genetic research on the influenza virus in India. The lack of genetic surveillance data on influenza in India raises a larger question about infectious diseases surveillance.
One of the main challenges for surveillance of infectious diseases in India is lack of reporting from the private healthcare sector, which delivers healthcare to more than 75% of the population. It is imperative to incorporate the private health sector in disease surveillance programs, without which there will be severe under-reporting of cases. A clear cut example is under-reporting of cases in Tuberculosis. India has the highest burden (2 million new cases estimated) in the world and a recent report published in the Lancet Infectious Diseases journal revised the country’s Tuberculosis case burden to an additional 2.2 million cases every year (14). Private healthcare sector is usually the first point of contact for several of these patients, therefore a vital link in the disease control mechanism. A robust and an easy-to-use web based or a mobile based surveillance system can be a boon for the country’s disease surveillance program. In addition, adequate measures to improve education and awareness among the private healthcare providers should also be ensured.
Whilst there has been considerable progress in developing India’s health system in recent years, including the establishment of their Integrated Disease Surveillance Programme (IDSP) in 2004, there are still critical health systems gaps to address in public health and infectious diseases (12). Travel and globalisation mean that infectious diseases spread around the world rapidly, and that all countries must be prepared for epidemics. Research done at UNSW showed that the country of greatest risk of importation of MERS coronavirus from the Middle East is India, because of the large number of Haj pilgrims from India. The epidemic of MERS in South Korea which resulted from a failure to screen for MERS when a return traveller presented to hospital, highlights the global nature of epidemics. There is a need for developing better capacity to respond to large-scale epidemics, epidemiological capacity to analyse outbreaks, an increased pool of skilled public health practitioners in India, and laboratory capacity to appropriately diagnose diseases (12). All of these challenges are indeed opportunities to improve disease surveillance, response capacity and preparedness for epidemics in India.


Adverse consequences of such epidemic outbreaks are :
1. loss of life ,
2. Loss of income
3. Economic burden on family , society and country
4. Working hours lost
5. Expenditures increases
6. Impact on society
7. Impact on economy
8. Impact on environment
9.
Measures adopted to cure epidemic and pandemic:
The two principal strategies for containing serious human outbreaks of influenza are therapeutic countermeasures (e.g., vaccines and antiviral medications) and public health interventions (e.g., infection control, social separation, and quarantine). Many of the barriers to effective interventions are technical and have been thoroughly discussed. This article focuses on the formidable legal and ethical challenges, which have yet to receive sufficient attention.
Industrialized countries place great emphasis on scientific solutions. Vaccination and, to a lesser extent, antiviral medication are perhaps the most important medical interventions for reducing morbidity and mortality associated with influenza. Given the limits of medical countermeasures, a broad range of public health would likely be employed against an influenza pandemic, from relatively innocuous techniques, such as disease surveillance and hygienic measures, to considerably more restrictive interventions, such as social distancing, travel restrictions, quarantine, and case isolation. There are reasons to believe that all of these will be effective to at least some degree.




No comments:
Post a Comment